When to Start Pumping: Building Your Breast Milk Supply
Breastmilk is the gold standard for infant nutrition as it is uniquely tailored to meet the developmental needs of the neonate. A common concern for breastfeeding mamas is low milk supply as many feel that they are “just making enough”. What this really means is that your body is dialed into your baby’s specific needs and making the perfect amount. Still, having little or no milk stored can be stressful for times when mother is away. Building a small stash can be helpful and a huge relief.
When to Start Pumping: Understanding Your Milk Supply
First, we need to understand how milk production works. During pregnancy progesterone is produced by the placenta and helps limit breastmilk production. After the baby is born and the placenta is delivered, progesterone levels rapidly drop and allows for lactation to begin.
Prolactin and oxytocin are two hormones involved in milk production. Prolactin also increases during pregnancy and stimulates breast development and milk production. Levels spike immediately after birth and then begin to rise and fall in response to nipple stimulation (breastfeeding, hand expression, or pumping). Prolactin follows a circadian rhythm with levels being higher at night, so do not skip out on those night feeds!
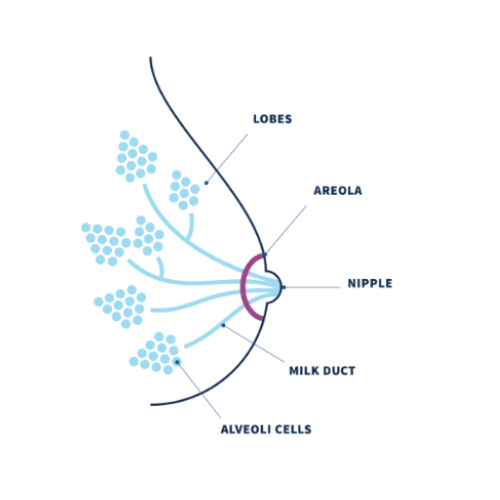
Oxytocin, also known as the love hormone, stimulates the milk-ejection reflex or “letdown”. It causes contractions that force milk from the alveoli into the ducts, which then flows to the nipple to be available for baby during feedings. Some moms feel a tingling or pulling sensation during let down. Oxytocin also helps control postpartum bleeding by stimulating uterine contractions and aids in uterine involution (shrinking).
Remove milk often!
Milk production slows when the breasts are full due to a mechanism called the “Feedback Inhibitor of Lactation” (FIL). This is why it is so important to frequently empty the breast for a robust milk supply. If you wait until your breasts feel full before feeding or pumping, over time your milk supply will gradually reduce to the reduced demand.
Colostrum
Colostrum is the first milk produced starting during pregnancy and continuing through the first few days of postpartum. Commonly referred to as “liquid gold” for its rich yellow hue, colostrum is densely packed with protein, immunoglobulins, and antioxidants. During this initial phase, milk volume is intentionally low, perfectly matched to the newborn’s small stomach capacity. Around days 2 to 5 milk volume begins to increase causing breast fullness and engorgement.
Fun fact: Did you know that breast size has nothing to do with milk production capacity? Small-breasted people can often produce just as much milk as those with larger breasts!
When to Start Pumping: Different Scenarios
The big question is... when should YOU start?
Short answer: It depends! Every mother-baby duo is unique, so let's break it down based on your specific situation.
Healthy, Full-term Babies who are Nursing Well:
If your baby is full term and nursing effectively, wait until breastfeeding is well established (around 4-6 weeks) before introducing pumping. This allows time to establish a good latch, learn your baby’s hunger cues, and let your milk supply regulate naturally. Pumping too early may lead to oversupply, increased engorgement, and added maternal mental stress – time, cleaning.
Signs that breastfeeding is “well-established” :
Baby is gaining weight appropriately
Good wet and dirty diapers (least 6 wet diapers daily)
Nursing is comfortable and pain-free
Baby appears satisfied after feeds
Exclusively Pumping Mother:
If you plan to exclusively pump, you will begin pumping and hand expressing immediately after birth. Early stimulation is essential for initiating and building that milk supply.
Premature, NICU, and Hospitalized Babies:
Mothers of premature, NICU, or hospitalized babies, pumping also begin pumping within hours of birth using a hospital-grade breast pump. Start with hand expression in the first hour after birth and put baby to breast if possible. Seek help from hospital nurses and lactation consultants. Practice kangaroo care (skin-to-skin) when possible, to boost milk-producing hormones.
Babies Experiencing Latching Difficulty or Ineffective Nursing:
If your baby struggles to latch or isn’t transferring milk effectively, your body may not receive the signal to produce enough milk. In this case pumping may begin sooner than expected. Work closely with your medical team (pediatrician, lactation consultant, and dietitian) to develop a plan to establish and maintain a healthy milk supply while ensuring your baby receives adequate nourishment to grow.
How Often Do I Need to Pump?
Newborns feed 8-12 times a day. This is the same frequency that is needed to express milk to establish and maintain a milk supply. Exclusively pumping mamas will need to pump 8-12 times per day for about 15-20 minutes per session. Mothers doing a combination of feeding at the breast and pumping will only need to pump when a feeding is missed.
During the early weeks after birth it is very important for mothers to wake up and feed or pump to establish an adequate milk supply. Remember overnight is when those prolactin levels are their highest and if a mother skips a feeding the body will naturally down regulate supply.
When to Start Pumping: Plan for your Return to Work/School
Start building that stash a few weeks prior to the time that you will be away from your baby. In the United States the typical maternity leave is only 6-8 weeks, in which case pumping should begin around 4-6 weeks post-partum. Try adding a short pumping session (about 10 minutes) once a day immediately after a feeding, preferably the first early morning feeding when prolactin levels are still elevated. After doing this for a few days or weeks you can consider if adding a second pumping session would be beneficial. A good time to fit in a second session is immediately after feeding prior baby’s typical nap time.
Technically a mother only needs one day worth of pumped milk before returning to work, however a mother might feel more comfortable having at least a 3-day supply. What is a day supply? Consider how long you will be away from your baby and estimate how many bottles will be needed. Here is an example: A mother returns to work and is away from baby for 8-9 hours a day. A typical 3-month-old baby is likely drinking around 4 oz bottles and feeding every 3 hours. 12 oz of breastmilk will be needed for that first day away.
Create a personalized pumping schedule that fits your daily routine. Consider the times your baby would typically feed at home and plan your pumping sessions around those moments – aiming for consistent intervals, ideally every 3 hours. Shorter, more frequent sessions are more effective and less exhausting than skipping and trying to make up for it with a long 30+ minute pump. Consistency is essential for maintaining supply, so stick to your individualized schedule.
5 Tips for Effective Pumping
1. Select the right pump:
The pump should match your specific needs.
Tabletop pumps - High functioning pumps with lasting durability. Recommended for moms that are struggling with low supply, working moms, or exclusively pumping mamas.
Examples: Spectra S2, Motif Luna, or Cimilre S6
Portable pumps - Small yet powerful rechargeable pumps with added portability. These may have less setting options compared to tabletop pumps, but they are able to meet demands of frequent pumping. Great for moms that are always on the go and need a reliable and efficient pump to meet her lifestyle.
Examples: Zomee Z2, Motif Duo, Ardo Alyssa, Elvie Stride, and Baby Buddha
Wearable pumps - Feature a rechargeable pump with wearable cups that are discrete and convenient for maximum portability. These are ideal to ensure no pumping session is missed when on the go and pairs well when used with a primary.
Examples: Zomee Fit, Motif Aura Glow, and MomCozy S12
2. Proper Flange Fit:
Finding a flange size that fits your body will ensure comfort, maximize milk output, and reduce frustration. Check out our blog on how to find your ideal flange size and use our downloadable nipple measuring tool.
3. Try Hands-On Pumping:
This is a technique that a mom can use to massage her breasts before pumping to get the milk flowing. Then she can gently massage her breasts while pumping to help empty the breast. You can try warm compresses before and during pumping to promote increased milk flow.
4. Relax:
Oxytocin release (let down) occurs more easily for some moms when pumping in a comfortable and quiet place. You can also try looking at a photo or video of your baby to stimulate that “feel good hormone” and see the milk start flowing.
5. Replace pump parts regularly:
Pump parts wear out! Check the membranes and duckbills as these parts need regular replacement. Failing to replace worn out parts may reduce suction and cause less milk to be extracted. See Maternal’s quick guide on parts replacement.
The Bottom Line
Every parent and baby are different. What works for one might not work for another, so be gentle with yourself as you figure out your unique journey. Whether you pump occasionally, part-time, or exclusively, you're doing an amazing job providing for your little one!
Seeking Help with Your Milk Supply or Selecting a Breast Pump?
At Maternal by Sentido, we offer breast pumps through insurance with little to no cost out of pocket. After submitting the insurance eligibility form, we will quickly respond with the breast pump options your insurance covers. If you are not sure which breast pump is right for you, our experts will take the time to discuss your options and help you choose from one of our top-quality breast pumps.
After you place your order, your breast pump will be shipped directly to your home with no shipping cost.
After your breast pump order is submitted, you immediately qualify for complimentary lactation support whenever you need. Our certified Lactation Consultations will work with you directly to ensure a successful breastfeeding or pumping journey.
Connect with Maternal by Sentido
Our team is dedicated to providing the highest quality breast pumps through insurance and getting to know you as a mom and guiding you through your maternal health journey.
Maternal by Sentido has an online community offering informative blogs, downloadable material, and social media that will carry you through your maternal health journey.
References:
Wambach, K., & Spencer, B. (2021). Breastfeeding and Human Lactation. Jones & Bartlett Learning.
WIC Breastfeeding. Usda.gov. https://wicbreastfeeding.fns.usda.gov/
A Message from the Author:
Hi! I’m Tara. I am a wife, a mother of two energetic children, a registered dietitian, and a lactation consultant. As a lactation consultant, I specialize in helping mothers and babies navigate feeding and growth challenges. My mission is to foster a successful mother-baby dyad, understanding that every journey is beautifully unique. I am deeply committed to empowering mothers with the guidance, tools, and encouragement they need to thrive in their breastfeeding and parenting goals.
About the Author:
Meet Tara! Tara earned a Bachelor of Science in Human Food and Nutrition with a minor in Business Administration from the University of Houston, followed by a Master of Science in Nutrition from Texas Woman’s University. With over 17 years of experience in clinical nutrition, Tara has had the privilege of working with both adults and children. For the past six years, she has focused her expertise on pediatric nutrition at Texas Children’s Hospital in Houston, Texas, where she discovered her deep passion for supporting growing families. During this time, Tara earned her certification as a Certified Lactation Counselor (CLC) and later achieved the prestigious International Board Certified Lactation Consultant (IBCLC) credential. She accomplished this after completing over 1,000 hours of lactation-specific education and hands-on experience.